The World Well being Group estimates that roughly 280 million folks on the earth undergo from despair, the second high main reason for years lived with incapacity globally (International Burden Illness, 2019).
Not solely is despair frequent, however as much as 54% of sufferers who’ve skilled a depressive episode are prone to relapse (Bockting et al., 2015). Relapse is often outlined because the re-emergence of the preliminary episode of despair after some preliminary enchancment, whereas recurrence is the onset of a brand new episode of despair after restoration (Moriarty et al., 2021). Earlier research have explored pharmacological (Cipriani et al., 2018) and non-pharmacological methods (Buckman et al., 2018) to forestall each relapse and recurrence of despair.
It has been really helpful that psychological interventions must be delivered extra broadly throughout the globe, attempting to establish the individuals who could profit probably the most from these interventions (Patel et al., 2023). Nevertheless, the meta-analyses performed thus far have used mixture information, which don’t enable the stratification of therapy suggestions in line with particular person traits.
These limitations may be overcome – not less than partly – with a methodological method referred to as particular person participant information meta-analysis (IPDMA). Utilized by Breedvelt and colleagues (2024), IPDMA collects particular person information from every participant throughout the research included within the systematic evaluate, thus enabling the stratification of affected person subgroups and facilitating a extra correct evaluation of outcomes (Tudur Smith et al., 2016).

Not solely is despair frequent worldwide, however roughly 50% of sufferers who expertise a depressive episode are prone to relapse, making relapse prevention an essential space of analysis.
Strategies
The authors systematically searched (till January 2021) for randomised managed trials (RCTs) printed in 4 completely different digital databases to evaluate the efficacy of psychological interventions in stopping despair relapse and recurrence, evaluating Psychodynamic Psychotherapy, Cognitive-Behavioural Remedy, Mindfulness-Primarily based Cognitive Remedy, and Continuation Cognitive Remedy towards non-psychological interventions and treatment-as-usual (TAU).
For the statistical evaluation, a pairwise meta-analysis mannequin primarily based on IPD was adopted. Hazard ratio (HR) was chosen because the statistical measure to summarise time-to-event information. Because of the anticipated between-studies heterogeneity, a random-effects mannequin was used, and heterogeneity was assessed with I2 statistic. An inventory of predefined predictors and moderators from earlier research was used for multivariate mannequin analyses (Bockting et al., 2015; Buckman et al., 2018). Subgroup analyses had been carried out to match the efficacy of various psychological interventions.
Outcomes
This IPDMA included 14 research involving 1,720 sufferers with main despair. Members had been predominantly feminine (73%) with a mean age of 45.1 years and historical past of recurrent despair (common of 4.8 episodes, with 75% experiencing ≥3 episodes).
Sadly, details about essential medical and demographic traits was solely out there for the minority of members: as an example, ethnicity (29%), employment standing (56%), comorbid psychiatric situation (41%) or different medical situations (23%), psychological classes accomplished (49%), and former psychological intervention (55%) or treatment (23%).
The IPDMA confirmed that:
- Psychological interventions (as a gaggle) outperformed management situations in delaying the time to relapse accounting for a small heterogeneity (HR = 0.60, 95% CI [0.48 to 0.74], I2 = 14.9%) (please discuss with the graphic under).
- Including psychological interventions to TAU additionally diminished the chance of relapse compared with TAU (HR = 0.62, 95% CI [0.47 to 0.82], I2 = 28.3%) (please discuss with the graphic under).
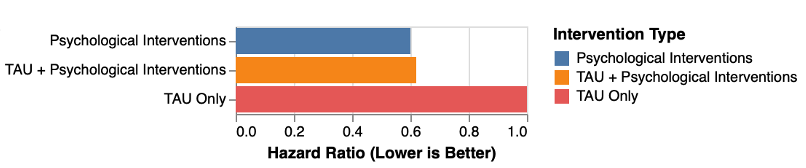
Comparability between completely different energetic methods in lowering the probability of relapse/recurrence of despair (Graphic created with RStudio by Rosario Aronica). View full size image
- Subgroup analyses discovered no distinction within the efficacy of various psychological intervention sorts to forestall despair relapse/recurrence, each when thought of as monotherapy and add-on therapy.
- The predictor evaluation discovered that having greater than two earlier depressive episodes (HR = 1.03, 95% CI [1.00 to 1.06]) and residual depressive signs at baseline (HR = 1.08, 95% CI [1.04 to 1.13]) can affect the chance of relapse within the management group.
- Moderator analyses revealed that members with three or extra earlier depressive episodes benefited extra from psychological interventions when in comparison with these with two or fewer episodes (HR = 0.55, 95% CI [0.37 to 0.79])
- Moderator analyses additionally confirmed that psychological interventions weren’t more practical in lowering relapse for these with two episodes or fewer when in comparison with TAU (two episodes, HR = 0.85, 95% CI [0.37 to 1.92]; one episode, HR = 1.48, 95% CI [0.40 to 5.53]).

This analysis highlights the potential superior efficacy of psychological interventions in stopping depressive relapse in comparison with management situations, particularly for sufferers who’ve skilled a number of earlier depressive episodes.
Conclusions
The findings from this IPDMA recommend that psychological interventions are efficacious in lowering despair relapse/recurrence danger, each as monotherapy and as add-on therapy.
These analyses recognized two potential predictors of the anticipated final result:
- Residual signs of despair at baseline, and
- Having skilled greater than two episodes of despair.
Regardless of the encouraging outcomes, replication research are warranted and warning is required earlier than these findings may be translated into medical observe. If there are sufficient research and out there information, it could even be essential to hold IPD community meta-analyses, to make clear the precise results of particular person psychological remedies and rank them primarily based on their efficacy and tolerability profile.

Regardless of the encouraging outcomes from Breedvelt et al. (2024), warning is required earlier than translating them right into a medical framework, and additional analysis is warranted.
Strengths and limitations
This research was carried out by a world-class staff of researchers and clinicians with experience in depressive issues and proof synthesis. The authors must be complimented for such an essential effort: amassing and harmonising particular person information from trials is all the time a big and complex process.
The most important energy of this research lies within the inclusion of IPD inside the meta-analysis framework. This method allows gathering demographic and medical information from members throughout all of the included research, and in addition permits the identification of potential predictors and moderators of the outcomes (Huang et al., 2016). Predictors and moderators discover the between-individuals variance of therapy response, however they’re fairly completely different. Predictors are used to find out which affected person could profit probably the most from a given therapy, whereas moderators reveal which traits render a specific therapy more practical than one other for a given affected person (Vousoura et al., 2021).
Authors adhered to the PRISMA-IPD reporting requirements tips (Stewart et al., 2015), and pre-registered the research protocol on PROSPERO.
As all methodological approaches, IPD meta-analyses have some limitations. Considered one of these is the problem to retrieve IPD from earlier trials, as skilled by Breedvelt and colleagues who managed to get entry solely to 18 out of the 28 trials recognized. Moreover, the incompleteness of the dataset, significantly by way of demographic and medical data, represents an extra weak point, which limits the exterior validity of the findings.
As reported within the IPDMA protocol, the authors used some strict choice standards for his or her evaluation: time to follow-up restricted to 12 months, the exclusion of research not measuring time to relapse, and the exclusion of naturalistic research on the long-term impact of energetic interventions. This method, whereas meant to mitigate bias and improve inside validity, could have an effect on the generalisability of findings, doubtlessly limiting the usage of these information to broader medical contexts.
Furthermore, though a risk-of-bias evaluation instrument was employed to guage the standard of the included research (Furlan et al., 2015), the latest Cochrane tips encourage the adoption of the Threat-of-Bias evaluation instrument 2 (RoB 2) (Sterne et al., 2019). This up to date framework affords a extra granular evaluation per final result, fairly than per research, permitting a greater understanding of certainty of proof.

Particular person participant information (IPD) meta-analyses are restricted by the problem of retrieving IPD from present trials, and by the quantity of lacking data within the datasets out there.
Implications for observe
From a medical perspective, this research solutions many questions and suggests new ones:
- Is (psychological) therapy indicated after a depressive episode? In that case, which method must be adopted and for a way lengthy?
- Are completely different psychological approaches equally efficient throughout the affected person populations?
- Can we tailor interventions to subgroups of sufferers who usually tend to profit from psychological remedies?
The findings from Breedvelt et al. (2024) on psychological interventions affords promising insights for medical utility, suggesting that psychotherapies are efficient in stopping depressive relapse (and recurrence) for a selected subgroup of sufferers. Ought to future research with broader and extra numerous affected person cohorts validate these findings, the implications will likely be important, significantly for clinicians coping with sufferers preferring to not take pharmacological interventions.
This research can present useful methods for medical observe: it identifies predictors of relapse and recurrence, providing clinicians potential medical biomarkers for affected person stratification. Such personalised approaches assist the shift from a one-size-fits-all method in the direction of extra personalised care: the fitting therapy for the fitting affected person on the proper time. Accounting for particular affected person’s wants, preferences, and dangers, this mannequin underscores the significance of a person-centred method by way of shared choice making.

The research by Breedvelt and colleagues is a crucial contribution within the subject of precision psychological well being, the place researchers and clinicians goal to focus on therapy to particular person sufferers bettering outcomes and lowering the incapacity and international burden of despair.
Assertion of pursuits
Andrea Cipriani and Rosario Aronica work within the Division of Psychiatry, College of Oxford the place one of many authors (Professor Willem Kuyken) of this manuscript additionally works; nonetheless, this weblog was drafted independently by the 2 authors.
Main paper
Breedvelt, J. J., Karyotaki, E., Warren, F. C., Brouwer, M. E., Jermann, F., Hollandare, F., … & Bockting, C. L. (2024). An individual participant data meta-analysis of psychological interventions for preventing depression relapse. Nature Psychological Well being, 1-10.
Different references
Bockting, C. L., Hollon, S. D., Jarrett, R. B., Kuyken, W., & Dobson, Okay. (2015). A lifetime approach to major depressive disorder: The contributions of psychological interventions in preventing relapse and recurrence. Scientific Psychology Assessment, 41, 16-26.
Buckman, J. E. J., Underwood, A., Clarke, Okay., Saunders, R., Hollon, S. D., Fearon, P., & Pilling, S. (2018). Risk factors for relapse and recurrence of depression in adults and how they operate: A four-phase systematic review and meta-synthesis. Scientific Psychology Assessment, 64, 13-38.
Cipriani, A., Furukawa, T. A., Salanti, G., Chaimani, A., Atkinson, L. Z., Ogawa, Y., … & Geddes, J. R. (2018). Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: A systematic review and network meta-analysis. The Lancet, 391(10128), 1357-1366.
Furlan, A. D., Malmivaara, A., Chou, R., Maher, C. G., Deyo, R. A., Schoene, M., … & Van Tulder, M. W. (2015). 2015 updated method guideline for systematic reviews in the Cochrane Back and Neck Group. Backbone, 40(21), 1660-1673.
GBD 2019 Psychological Issues Collaborators. (2022). Global, regional, and national burden of 12 mental disorders in 204 countries and territories, 1990–2019: A systematic analysis from the Global Burden of Disease Study 2019. The Lancet Psychiatry.
Huang, Y., Tang, J., Tam, W. W., Mao, C., Yuan, J., Di, M., … & Yang, Z. (2016). Comparing the overall result and interaction in aggregate data meta-analysis and individual patient data meta-analysis. Medication (Baltimore), 95(14), e3312.
Moriarty, A. S., Meader, N., Snell, Okay. I. E., Riley, R. D., Paton, L. W., Dawson, S., … & McMillan, D. (2022). Predicting relapse or recurrence of depression: Systematic review of prognostic models. The British Journal of Psychiatry, 221(2), 448-458.
Web page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., … & Moher, D. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ, 372.
Patel, V., Saxena, S., Lund, C., Kohrt, B., Kieling, C., Sunkel, C., … & Herrman, H. (2023). Transforming mental health systems globally: Principles and policy recommendations. The Lancet, 402(10402), 656-666.
Shinohara, Okay., Efthimiou, O., Ostinelli, E. G., Tomlinson, A., Geddes, J. R., Nierenberg, A. A., … & Cipriani, A. (2019). Comparative efficacy and acceptability of antidepressants in the long-term treatment of major depression: Protocol for a systematic review and network meta-analysis. BMJ Open, 9(5), e027574.
Simmonds, M. C., Tierney, J., Bowden, J., & Higgins, J. P. T. (2011). Meta-analysis of time-to-event data: A comparison of two-stage methods. Analysis Synthesis Strategies, 2, 139-149.
Sterne, J. A., Savović, J., Web page, M. J., Elbers, R. G., Blencowe, N. S., Boutron, I., … & Higgins, J. P. (2019). RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ, 366.
Stewart, L. A., Clarke, M., Rovers, M., Riley, R. D., Simmonds, M., Stewart, G., & Tierney, J. F. (2015). Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. JAMA, 313(16), 1657-1665.
Tudur Smith, C., Marcucci, M., Nolan, S. J., Iorio, A., Sudell, M., Riley, R., … & Williamson, P. R. (2016). Individual participant data meta-analyses compared with meta-analyses based on aggregate data. Cochrane Database of Systematic Opinions, 9(9), MR000007.
Vousoura, E., Gergov, V., Tulbure, B. T., Camilleri, N., Saliba, A., Garcia-Lopez, L., … & Poulsen, S. (2021). Predictors and moderators of outcome of psychotherapeutic interventions for mental disorders in adolescents and young adults: protocol for systematic reviews. Systematic Opinions, 10, 1-14.
World Well being Group. (n.d.). Despair. https://www.who.int/news-room/fact-sheets/detail/depression
Zhou, X., Teng, T., Zhang, Y., Del Giovane, C., Furukawa, T. A., Weisz, J. R., … & Xie, P. (2020). Comparative efficacy and acceptability of antidepressants, psychotherapies, and their combination for acute treatment of children and adolescents with depressive disorder: A systematic review and network meta-analysis. The Lancet Psychiatry, 7(7), 581-601.
